Medical and Health Care Professionals
Considerations and Resources for Providers who Provide Care to Displaced Patients
There may be situations that result in patients who are prescribed controlled substances abruptly losing access to care. It is important for displaced patients to re-stablish care quickly due to risk of severe medication withdrawal or turning to other sources, which make increase risk for overdose. View important
considerations and resources that providers may utilize to provide safe and effective care.
Information on Misapplications
December 2019:
A message was sent to all Pennsylvania prescribers to raise awareness of common misapplications of the Centers for Disease Control and Prevention and Pennsylvania opioid prescribing guidelines and the PDMP system.
Guide for Appropriate Tapering or Discontinuation of Long-Term Opioids Use
Once a patient is on opioids for a prolonged duration, any abrupt change in the patient's regimen may put the patient at risk of harm and should include a thorough, deliberative case review and discussion with the patient. This Guide provides advice to clinicians who are contemplating or initiating a change in opioid dosage. View the
Guide for Appropriate Tapering or Discontinuation of Long-Term Opioid Use (U.S. Department of Health & Human Services).
Centers for Disease Control and Prevention (CDC) research indicate that both fatal and nonfatal benzodiazepines overdoses increased from 2019 to 2020. Over 90% of all prescription and illicit benzodiazepine-involved overdose deaths also involved either prescription or illicitly manufactured opioids, highlighting the dangers of co-using opioids and benzodiazepines. Providers who are also considering benzodiazepine tapering may view
Addressing Benzodiazepine Overuse Summary Brochure (Alosa Health) and
Tapering Tool (Alosa Health).
Educational Information for Healthcare Providers
The Pennsylvania Department of Health has encouraged an opioid stewardship program in Pennsylvania which helps ensure that medical professionals have all the
education and training they need to effectively prescribe opioids and treat pain not just with opioids, but through alternative pain management treatment methods as well.
In addition, a collection of
clinical resources for healthcare providers houses a variety of resources focused on approaches to safer opioid prescribing, strategies for effective communication with patients, and more.
Naloxone for Your Patients
In March 2023, the U.S. Food and Drug Administration approved 4 milligram (mg) naloxone hydrochloride nasal spray for over-the-counter (OTC), nonprescription use. The change allows for this life-saving medication to be more readily available across many settings. Providers are encouraged to consider steps to standardize naloxone education and distribution in their practices and have multiple opportunities to promote free or low-cost naloxone to patients.
- The Pennsylvania Department of Health's Physician General signed a standing order prescription for naloxone, which means patients do not need a prescription from their provider.
- Pennsylvania residents who purchase naloxone using their insurance might be eligible to receive up to $50 to assist with the out-of-pocket cost. Patients may visit their local pharmacy to learn more about the Naloxone Copay Assistance Program.
- If a patient does not have health insurance or if cost is a barrier, they may be able to receive free naloxone by mail. Through a partnership with the Pennsylvania Commission on Crime and Delinquency and NEXT Distro, anyone can get naloxone mailed to their home for free. Learn more about free naloxone by mail.
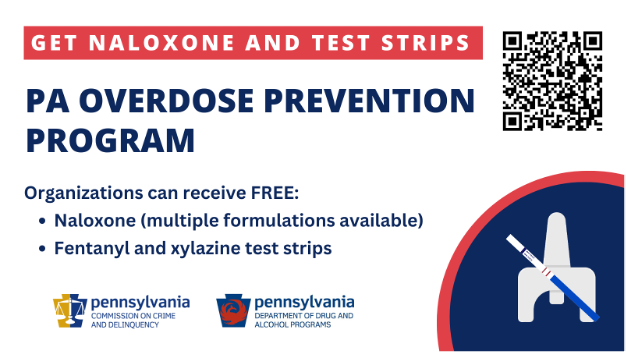
- In 2023, the Pennsylvania Overdose Prevention Program (POPP) was launched as a joint initiative between the Pennsylvania Commission on Crime and Delinquency (PCCD) and the Pennsylvania Department of Drug and Alcohol Programs (DDAP). This program offers multiple formulations of naloxone as well as drug checking strips designed to detect xylazine and fentanyl at no cost to organizations across Pennsylvania. One goal of this program is to increase community-based distribution, particularly among people who are currently using substances or people who know someone currently using substances. Healthcare organizations may make a request to receive FREE supplies using the POPP Request Form. Questions? Email: ra-cdpa-overdoseprev@pa.gov.
Report on Pain Management Best Practices
The Pain Management Best Practices Inter-Agency Task Force was convened by the U.S. Department of Health and Human Services in conjunction with the U.S. Department of Defense and the U.S. Department of Veterans Affairs with the Office of National Drug Control Policy to address acute and chronic pain in light of the ongoing opioid crisis. The Task Force emphasizes the importance of individualized patient-centered care in the diagnosis and treatment of acute and chronic pain. View the
Report on Pain Management Best Practices: Updates, Gaps, Inconsistencies, and Recommendations (U.S. Department of Health and Human Services).
Provider Clinical Support System
The
Provider Clinical Support System, or PCSS, is a program funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) to train primary care providers in the evidence-based treatment of chronic pain and prevention and treatment of substance use disorder.
The
PCSS clinical mentoring program is a national network of trained clinicians with expertise in treating substance use disorder, co-occurring mental disorders, and pain management. There are three mentoring options available for health professionals who prescribe opioids for pain or treat individuals with substance use disorder: 1) post clinical questions to an online discussion forum and receive answers from experts, 2) directly submit a clinical question and receive a prompt response via email, or 3) request a mentor to be "matched up" with an expert in their region who can provide one-on-one guidance and support.
PCSS has also developed
education and training resources for healthcare providers on topics such as
treating patients who suffer from chronic pain,
minimizing distress during tapering,
screening, brief intervention, and referral to treatment (SBIRT) for SUD in primary care settings, and
Medications for Opioid Use Disorder (MOUD).
Non-Opioid Directive
There are an estimated 1.2 million Pennsylvanians in recovery from substance use disorder (SUD) and SUD affects one in four Pennsylvania families. Stigma, shame, and related communication barriers can create an unnecessary risk of relapse or recurrence of substance use behaviors.
The
Pennsylvania Non-Opioid Directive is a form that patients may complete to communicate to their healthcare provider that they do not wish to be offered, supplied, prescribed, or otherwise administered any controlled substance containing an opioid. This tool helps prescribers and patients begin a dialogue about substance use history and it may prevent a provider from inadvertently prescribing opioids to those who could be adversely affected.